For anyone who has to care for a loved one or client during the bathroom routine, we can greatly help the individual by staying open minded and accommodating to the approach taken. It’s important not to get caught up on perfection instantly, but reassuring the individual that they can share their feedback and preferences to refine the bathroom process so they feel like they’re being respected.
In this article we’re going to talk about the idea of bathing etiquette – how can family, carer, OT and anyone else who helps an individual feel like bathing is something they’re in control of? Here’s just a few thoughts for our readers to ponder.
Determine what the bathing plan is ahead of time
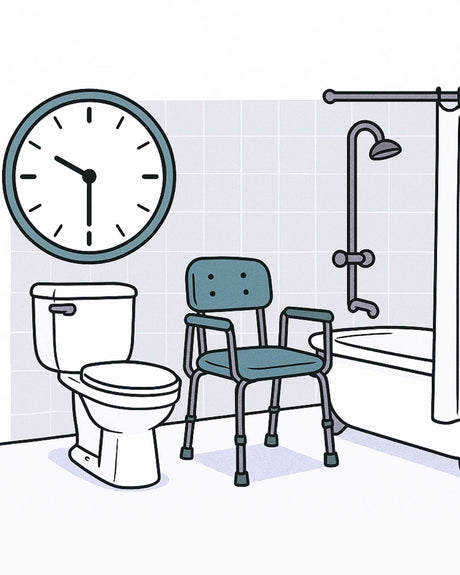
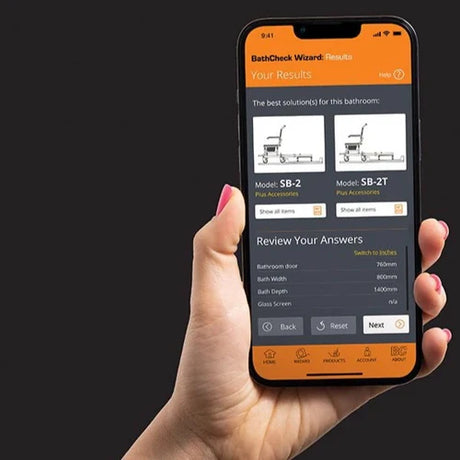
First, it’s a priority to understand how the individual with the mobility challenges wishes their bathing to proceed. Doing so means that family or carer can start to plan with the OT what equipment is needed, and what functions they’ll ultimately need to provide.
The plan for bathing should be captured by the OT and everyone should be aware of how things will go, right from waking up through to exiting the bathroom to get dressed.
Preparing for bathing and undressing
Allowing solo bathing as much as possible
Imagine the difference between bathing in front of someone else, vs. having that 5 or so minutes to yourself to enjoy a warm shower. We think everyone deserves that, and if it’s possible – it should be part of the plan if the individual wishes!
Of course, in all these situations, it’s important to defer ultimately to the occupational therapist’s expertise. If they deem it a risk to the personal safety of the mobility impaired person to bathe alone, there may need to be another plan in place – does the equipment need to be upgraded, can other parts of the process be done alone? It’s the OT’s job to find answers to these questions and guide families accordingly.
High communication around bathing
If the individual is 100% communicative with no barriers, then achieving good bathroom etiquette is much easier. They can adjust the routine as they see fit or ask for help should they need.
Leaving the individual alone for toilet use if possible

Protecting modesty when transferring between bathroom and bedroom

Using equipment that can provide more dignity for individuals
Further reading
Enjoyed this article? You may be interested in these resources online:
- Families supporting a disability – Showerbuddy
- Safe Patient Handling At Home – How carer and individual work together
- The Relationship Between Being Respected and Quality of Life of Disabled People – Carl Friedman, The Council on Quality and Leadership via Disability Studies Quarterly




























![Toilet Training A Young Child With Mobility Challenges [And How A Shower Chair Can Help]](http://shower-buddy.com/cdn/shop/articles/toilet-training-disabled-child_520x500_a90e5234-d372-435d-aa56-8da15dd3836c.webp?v=1722557239&width=460)



















