Note: This article provides information specifically about bathroom mobility and how it relates to muscular dystrophy. For more information on MD specifically, please consult your local health authorities.
Muscular Dystrophy, which weakens particular skeletal muscles can manifest in a number of ways, presenting as impairment to specific sets of muscles. This can render someone with MD unable to use the bathroom independently. As muscular dystrophy is typically progressive, we often work with users who have to navigate degrading levels of mobility which can be very challenging.
Today we want to touch on the bathroom experience for someone with muscular dystrophy and how those around them can best support their evolving needs with bathing and toileting.
Understanding the particular type of muscular dystrophy
As muscular dystrophy varies in how it affects muscle areas, it’s important to have a clear assessment of this before proceeding with a plan to manage around the home. Health professionals will provide a detailed diagnosis which can then be supplied to the occupation therapist (OT) to start a support plan.
Common types of muscular dystrophy include Becker and Duchenne. For MD that impacts arms and leg use, assistance in the bathroom is commonly needed.
Tapping into support available in your area
Muscular dystrophy is a fairly common occurrence, with 1 in 3,500 male births worldwide having Duchenne muscular dystrophy (DMD). Health systems are therefore well versed in this genetic condition and a number of supports are available depending on where you live. Your personal doctor will be able to refer you or your loved one to this support. This can include groups and networks, medical professionals and of course OTs to help plan and live daily life.

Family, friends and the MD community
Coping with the challenges of muscular dystrophy shouldn’t be faced alone. The support of family both physically and emotionally is a huge part of an individual’s journey. Friends and others facing MD are also important to share experiences.
When it comes to matters as private as using the toilet or bathing, family members should work alongside their loved one, finding solutions that maintain dignity and comfort during these tasks.
Establishing level of independence vs. support required
The bathroom, with its hazards and reliance on stable body position during washing up, bathing and toileting makes muscular dystrophy a significant barrier towards independence.
Part of the OTs assessment is to determine what degree of mobility the individual has. It’s important that a plan provides all the support needed, without removing independence that the individual with MD otherwise is capable of maintaining. That’s why it’s so important for this stage to be a collaborative process between health professionals, OT, family and the person with the condition.
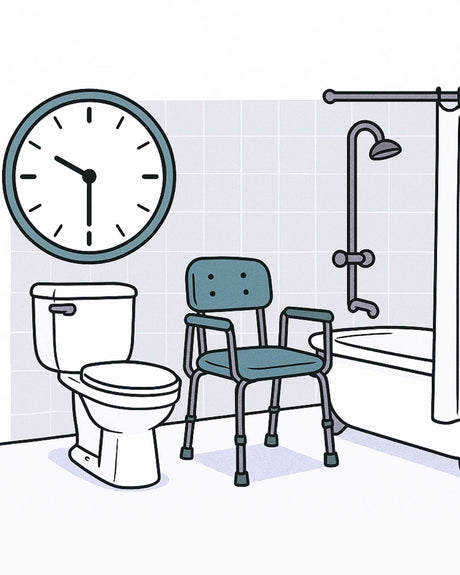
Using the bathroom may be possible with a degree of independence, such as bathing oneself but needing help getting in and out of the shower. Or, the effects of muscular dystrophy may necessitate a complete support from start to finish. Whatever the requirements, any leg or arm mobility challenges may mean the individual is a candidate for a shower chair or other support equipment.
A bathroom plan needs to stay dynamic and reviewed regularly
With a progressive condition like MD, the plan for bathroom mobility must be an ongoing discussion. Communication between individual, carer and health providers like the OT can ensure that adjustments are made when mobility changes.
How well the plan is working will depend on:
- The individual’s ability to conduct personal activities like bathing and using the toilet alone.
- Whether the individual can support their own weight and remain stable in certain positions.
- Whether they have the ability to move their legs, particularly if using a bathtub style shower.
- How much of a role does equipment play in the transfer and mobility in the shower.
- The individual’s own comfort and satisfaction with the current bathroom plan.
These factors will evolve over time, so it’s important that regular check ins happen with the OT.
Assessing the bathroom’s fit for purpose
An OT will conduct an assessment on the bathroom against the required support plan. Some bathrooms are not naturally laid out for someone with mobility needs like muscular dystrophy. Historically modifying the bathroom required expensive remodeling, making many rented houses very difficult to accommodate those with impairments. Now, with solutions like Showerbuddy, excellent bathroom mobility support is possible.
We work with OTs and their clients with muscular dystrophy frequently to help ascertain if a bathroom is fit for our mobility solutions – in most cases they are, but we can help determine what shower chair and accessories will be needed to enable the user the best possible experience.

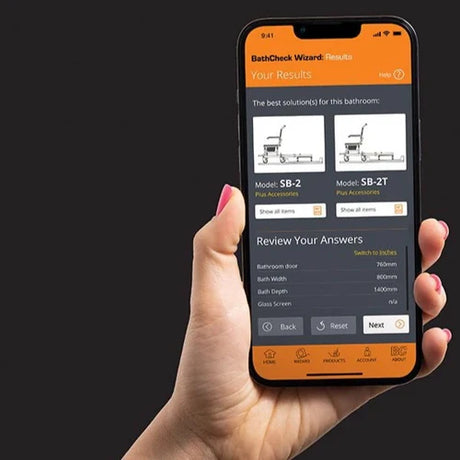
Showerbuddy is a partner to OTs and distributors as they assess bathrooms. So much so, that we developed an industry-leading app called BathCheck. This app, available for mobile and via the web, guides the measurement of a bathroom to ensure the best possible solution for the user.
Shower equipment that evolves with the user
Those living with MD will need their equipment to keep up with their changing mobility needs. That’s why a shower chair system should be able to grow with the user, have a good degree of adjustment and offer a host of accessories. A shower chair may start as simply seated support for a user able to bathe themselves with hand and arm mobility, then be adapted to provide full body support as a carer assists with the transfer in and out of the shower and bathing itself.
The benefits of a full transfer system like Showerbuddy is that it provides complete support with no manual lifting between toilet, shower and other activities.
Further Reading
- Duchenne Muscular Dystrophy – Rare Diseases
- Living with Muscular Dystrophy – CDC.gov
- Toileting & Showering – Parent Project Muscular Dystrophy




























![Toilet Training A Young Child With Mobility Challenges [And How A Shower Chair Can Help]](http://shower-buddy.com/cdn/shop/articles/toilet-training-disabled-child_520x500_a90e5234-d372-435d-aa56-8da15dd3836c.webp?v=1722557239&width=460)



















