By Barry Redican, Showerbuddy CEO
A step-by-step OT guide to assessments, photos, functional wording, and evidence.
In this issue 3 of Access Insights, we break down how to structure strong clinical reasoning to strengthen your funding case.
Our goal is simple: to give OT’s practical, evidence-driven tools that help you achieve faster, more confident bathroom outcomes for your clients
The OT Clinical Reasoning Framework for Bathroom AT
Effective justification for bathroom Assistive Technology (AT) relies on clear, structured clinical reasoning. Assessors across NDIS and Support at Home consistently indicate that approvals are more likely when OT's explicitly describe the functional problem, the contributing impairment, the associated risk, and the way the proposed AT resolves the issue. The following framework provides a practical method you can use for any bathroom assessment.
1. Describe Functional Capacity in the Bathroom
Rather than describing a diagnosis or symptom, describe what the client can and cannot do during the specific bathroom task.
Focus on:
- Balance (static and dynamic)
- Transfers (onto toilet, into shower, over hob, onto bath board, etc.)
- Reach & grasp (shower controls, grab rails, towel bars)
- Endurance & fatigue
- Cognition (sequencing, safety awareness, impulsivity)
- Carer requirements (two-person assist, manual handling risk)
Example wording: “Client is able to stand for less than 10 seconds unsupported and requires upper-limb support to step over a 200mm shower hob. Reduced ankle dorsiflexion and reduced dynamic balance result in unsteadiness during transfers. Client cannot safely pivot or reorient within the shower space without carers assistance.”
This demonstrates functional limitation, not diagnosis.
2. Link Impairment → Task → Risk → Solution
Assessors respond very well to a clear causal chain.
Step-by-step format:
1️⃣ Impairment
What physical or cognitive limitation is present?
2️⃣ Impact on Task
What part of the bathroom task is affected?
3️⃣ Risk
What is the immediate or potential safety consequence?
4️⃣ Solution
How the recommended AT removes or reduces that risk

💦 Example:
Impairment: Reduced lower-limb strength, poor dynamic balance, and reduced load-bearing capacity through the right arm.
Impact on Task: Client is unable to safely step into the shower and cannot perform a controlled sit-to-stand from a low surface.
Risk: High risk of falls during entry, standing tasks, and washing lower limbs. Carer is required to physically stabilise client, creating manual handling risk.
Solution: Showerbuddy transfer system provides seated transfer into the shower without stepping over the hob. Client remains fully supported, eliminating standing tasks and reducing carer involvement from physical sprain assistance to supervision and light assistance only.
This structure shows exactly why the AT is appropriate, safe, and preferable to home modifications.
3. Example Justifications That Succeed
These are based on real patterns in assessor feedback (NDIS, SaH, DVA, and insurer pathways).
⭐ Justification Example 1 — Falls Risk
“Client has had two near-falls when stepping over the 180mm shower hob due to impaired balance and left knee instability. A Showerbuddy system provides seated transfer, removing the requirement to step over the hob and significantly reducing fall risk. Home modifications were considered but would not address the client’s need for supported, seated showering.”
⭐ Justification Example 2 — Carer Burden
“Current showering requires one carer to support balance and another to manage washing tasks. This creates unsustainable manual handling demands. A transfer system supports the client in a stable seated position, allowing a single carer to assist safely, reducing load and long-term injury risk.”
⭐ Justification Example 3 — Cognitive Impairment
“Due to reduced sequencing and poor hazard awareness, client cannot follow safe instructions for stepping into the shower. The recommended AT eliminates the need for standing transfers and reduces environmental hazards, allowing the carer to maintain control with minimal redirection.”
⭐ Justification Example 4 — When AT Is Better Than Home Mods
“Bathroom modifications were considered; however, removing the shower hob and enlarging the entry would require structural work, council approval, lengthy delays, and client displacement. The AT solution provides immediate safety, can be implemented within days, and meets all functional needs without construction.”
As an OT You Can Use This Framework Immediately
- Structure your report headings as: Impairment → Task → Risk → AT Solution
- Use clear functional descriptions (avoid medical terminology unless essential).
- Include photos highlighting barriers (shower hob, narrow entry, awkward reach).
- Note why home modifications are not the preferred solution.
- Refer to dry trial outcomes to strengthen justification.
Environmental Barriers:
How to Document & Photograph a Bathroom for Funding
- The 7 photos OTs should always take
- What assessors look for
- What not to send
Clear environmental documentation is one of the strongest contributors to a successful AT justification. Assessors rely on photos to understand the bathroom layout, hazards, and functional barriers you have described in the report. The goal is to help them see what you see — without overwhelming them with unnecessary images.

Below is a simple, evidence-focused photography framework specifically for bathroom AT cases.
The 7 Photos OTs Should Always Take
1️⃣ The Entry to the Bathroom
- Show doorway width, swing direction, and any lips or thresholds.
- Include mobility equipment (if used) in relation to the doorway.
Why it matters: Assesses accessibility, turning space, and doorway barriers.
2️⃣ Whole-Bathroom “Context” Shot
- A wide photo capturing toilet, shower/bath, vanity, and overall layout.
Why it matters: Helps assessors understand spatial relationships and movement patterns.
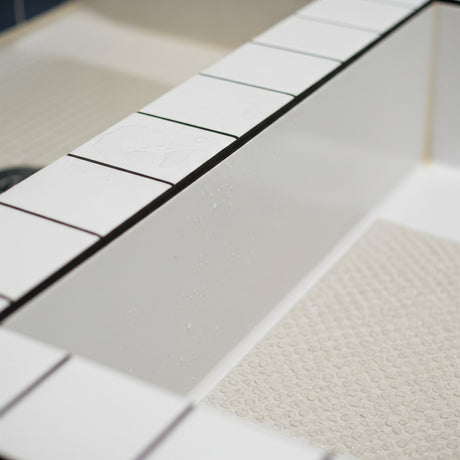
3️⃣ Shower Area — Full View
- Show the shower hob height, screen position, step-over hazards, and reach distances.
Why it matters: Demonstrates transfer challenges and trip/fall risks.
4️⃣ Inside the Shower — Functional Space
- Photo from inside the shower looking outward where possible.
- Capture turning space, grab rails (or lack thereof), and shower controls.
Why it matters: Shows why standing tasks may be unsafe or impossible.
5️⃣ Toilet Transfer Space
- Show side-access clearance, space for carer support, and height of seat.
Why it matters: Assists with determining whether AT or mobility support is needed.
6️⃣ Floor Levels & Slip Hazards
- Show wet-area transitions, tile lips, uneven surfaces, or puddling areas.
Why it matters: Assesses fall risk and determines suitability of seated vs standing tasks.
7️⃣ The Client’s Typical Position
- Demonstrate where the client stands/sits (with consent), or use equipment/chairs as markers.
- Show reach to shower controls, grab rails, or supports.
Why it matters: Supports functional reasoning — not just environmental description.
What Assessors Look For in Bathroom Photos
✔ Evidence of functional difficulty
Photos should align with wording in the report:
- limited step-over clearance
- insufficient turning space
- unsafe reach to controls
- poor carer access
- height differentials
✔ Clear, uncluttered visuals
The assessor should immediately understand:
- the hazard
- the risk
- why the proposed Showerbuddy SB1 sliding transfer chair resolves it
✔ Confirmation that home mods may not be feasible
Visuals and descriptions highlighting:
- Structural walls, if one needs removal to create space
- Existing floor structure is difficult to form slope to a new shower drain
- Shower rebuild involves extensive waterproofing renewal
- Potential electrical issues, damage to underfloor heating
- Drainage needs an upgrade for wet room floor waste
- Single bathroom home – no facilities for client during construction
- Risk to client from construction dust, noise and upheaval
- Potential consenting and construction delays
- Body Corporate / Owners Corporation restrictions?

✔ Carer manual handling considerations
Photos that make obvious:
- lack of standing room
- need for bending, twisting, or lifting
- positions that place carer at risk of sprain and injury
These strengthen AT justification over home modifications.
🚫 What NOT to Send
✘ Too many photos
Avoid sending 20–30 images. This slows assessors down and weakens clarity.
Optimal: 7–10 strong photos.
✘ Photos without context
Close-ups of tiles, grout, or fixtures without explanation don’t add value.
✘ Poor lighting or blurry images
Dark, shadowed, or low-resolution photos reduce confidence in the assessment.
✘ Photos of the client in unsafe or undignified positions
Avoid:
- showering images
- minimal clothing
- unsafe setups staged for the camera
(Use a chair, marker, or OT demonstration instead.)
✘ Irrelevant rooms or angles
Only include spaces directly affecting showering, toileting, transfer, and mobility.
How You Can Use This Today
- Build a photo folder template for each assessment.
- Take the 7 essential photos as part of every bathroom visit.
- Use captions directly under each photo in the report.
- Align photos with the “Impairment → Task → Risk → Solution” reasoning framework from Section 1.
This creates a clean, assessor-friendly justification that speeds up decision-making and improves the likelihood of AT approval.
Examples that recommend Showerbuddy as an AT solution for that client…
“Of the available options, the Showerbuddy sliding transfer system offers the safest transfer method without requiring structural bathroom changes. It addresses the participant-specific risks identified (falls, step demarcation, carer strain), and represents the most cost-effective solution compared with home modifications.”
“A mobile shower/commode transfer system with sliding bridge is the least-intrusive and safest solution for this participant. Based on the participant’s mobility, carer requirements, bathroom layout, and the need to minimise manual-handling risk, the Showerbuddy system meets these requirements most effectively.”




























![Toilet Training A Young Child With Mobility Challenges [And How A Shower Chair Can Help]](http://shower-buddy.com/cdn/shop/articles/toilet-training-disabled-child_520x500_a90e5234-d372-435d-aa56-8da15dd3836c.webp?v=1722557239&width=460)



















