What are they and how to avoid them.

A practical, new-year checklist to strengthen assessments under NDIS & Support at Home
As we work within the biggest shift in funding structures in more than a decade, bathroom AT decisions will be under sharper scrutiny — not just what is recommended, but why.
OTs tell me that the New Year is a time when they want something simple, practical and easy to apply. So here’s a short, save-worthy checklist you can take into 2026.
These are five of the most common bathroom AT mistakes that lead to confusion, re-visits… and occasionally funding knockbacks. More importantly — here’s how to avoid them.
1. Recommending AT before fully understanding the carer situation
Bathroom safety is rarely just about the client. The carer load, injury risk, frequency of transfers, and bathroom layout all directly influence the AT choice.
The mistake
Jumping straight to equipment without documenting:
· How often the carer assists
· The carer’s physical capacity
· Whether carer strain has already occurred
· Whether the carer can safely step into or reach across the shower
How to avoid it
Include one short functional paragraph describing the carer’s involvement and risk. Funding bodies respond strongly to joint needs rather than client-only descriptions.
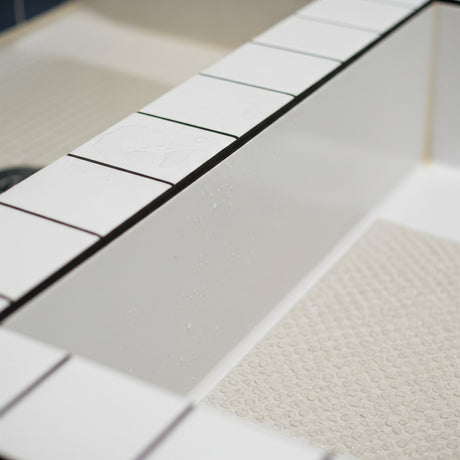
2. Taking photos that don’t show the real access problem
A surprising number of bathroom photos look “fine” — because the angle hides the issue.

The mistake
Photos that:
· Are taken too close
· Don’t show the full shower entry
· Hide the step height
· Crop the toilet, grab rails or wall distances
How to avoid it
Capture five must-have angles:
1. Full shower entry
2. Side view showing step or lip
3. Toilet space, including side transfer width
4. Overhead view showing layout
5. Any carer access difficulties
This alone reduces follow-up questions by more than half.
3. Using diagnostic language instead of functional language
Funding bodies do not fund conditions — they fund impacts and risks.
The mistake
Using phrases like:
· “Client has MS”
· “Client has reduced balance”
· “Client is a falls risk”
These statements don’t explain why AT is required.
How to avoid it
Use functional cause-effect wording:
“Client is unable to step into the shower due to left-sided weakness and requires carer support for safe transfer. Current method places the client at risk of knee collapse and the carer at risk of lumbar strain.”
That one sentence is far more powerful than a diagnosis.
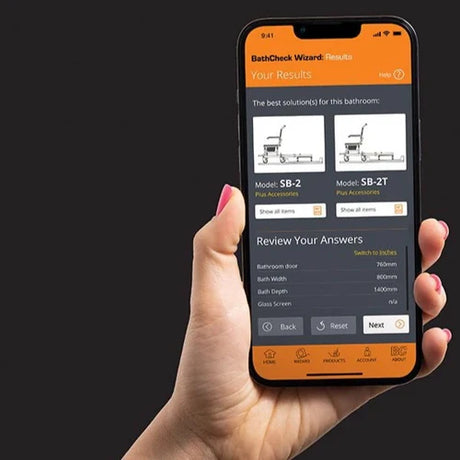
4. Recommending Home Mods when AT would solve the problem faster and more affordably
This is one of the biggest upcoming factors under Support at Home.

The mistake
Jumping to bathroom modifications when a transfer system would achieve:
· Faster installation
· Lower cost
· Less disruption
· Reduced manual handling risk
How to avoid it
Ask one simple question:
“Will AT solve the access limitation without structural change?”
If yes, the clinical justification is usually stronger for AT than for mods — especially when the remodel cost is 3×–4× higher.

5. Not clearly linking AT choice to specific functional outcomes
Funding decision-makers want to know why this item, not just any item.
The mistake
Recommendations that state only the product name, without describing:
· The exact functional improvement
· The safety gain
· The reduced carer risk
· The avoided cost (e.g., bathroom mod)
How to avoid it
Finish with a clear justification line:
“The recommended shower transfer system will allow safe seated access without stepping, eliminate carer lifting, and prevent falls during shower entry — outcomes not achievable with current equipment.”
This closes the loop beautifully.
🔎 Why these mistakes matter in 2026
With NDIS evolving and Support at Home enacted, clarity, function-first wording and evidence-backed recommendations will matter more than ever.
Getting these five areas right strengthens:
· The assessment
· The photos
· The functional wording
· The reasoning for AT vs mods
· The overall funding outcome
And it reduces repeat visits — something every OT appreciates in the New Year.
If you'd like a free checklist version of this for your team, message me.
You can also download the Checklist here… Free Checklist for OT's
Thank you for reading Access Insights.
My goal is to support therapists and to help clients stay safe at home — without the delays and confusion the system often creates. In researching this article and developing some images I also use AI.
Thank you for supporting Showerbuddy, the whole team is there to help you.
Barry Redican CEO — Showerbuddy
Contact us for any assistance or to arrange OT Training … admin@shower-buddy.com
Safe access. Smart design. Real independence.
#NDIS #SupportAtHome #OccupationalTherapist #Showerbuddy #AssistiveTechnology #AgedCare #BathroomSafety




























![Toilet Training A Young Child With Mobility Challenges [And How A Shower Chair Can Help]](http://shower-buddy.com/cdn/shop/articles/toilet-training-disabled-child_520x500_a90e5234-d372-435d-aa56-8da15dd3836c.webp?v=1722557239&width=460)



















