Red Flags That Make Standing Transfers Unsafe
When Standing Transfers Should Be Replaced with Seated Transfers
A growing theme in funding decisions and clinical risk reviews
Across Australia and New Zealand, a consistent pattern is emerging in funding panel feedback, incident investigations, and clinical risk reviews: standing transfers are being challenged earlier and more often—particularly where safer seated alternatives exist.
This issue explores when and why standing transfers should be replaced with seated transfer pathways, and how OTs can document and justify that transition effectively.
Why This Matters Now
Standing transfers are increasingly scrutinised because they:
· Rely heavily on variable human performance
· Fail suddenly when fatigue, illness, or cognition changes
· Transfer risk to both the client and the carer
· Are difficult to defend once a fall or near-miss has occurred
In contrast, seated transfer systems are being recognised as risk-mitigation equipment,
not simply mobility aids.

Red Flags That Make Standing Transfers Unsafe
Standing transfers become clinically inappropriate when any of the following are present—especially in combination:
Physical Red Flags
· Reduced lower-limb strength or asymmetry
· Knee buckling, joint instability, or pain on weight-bearing
· Poor trunk control or inability to maintain upright posture
· Reduced grip strength affecting rails or frames
· Delayed motor response or freezing episodes
Cognitive & Neurological Red Flags
· Inconsistent command following
· Reduced insight into limitations
· Parkinson’s, stroke history, MS, ALS or progressive neurological decline
· Fluctuating alertness (e.g. medication cycles, fatigue)
Environmental & Contextual Red Flags
· Wet bathroom floors or confined shower spaces
· Carers unable to maintain correct manual handling posture
· Transfers occurring multiple times per day
· Time pressure leading to shortcuts or unsafe techniques
Key insight: If a standing transfer requires perfect conditions to remain safe, it is no longer a robust solution.
Indicators a Client Needs a Seated Transfer Pathway
A seated transfer should be considered when:
· The client can sit reliably but cannot stand consistently
· Standing transfers require hands-on lifting or blocking
· Carers report anxiety, fatigue, or near-miss incidents
· Transfers deteriorate late in the day or during illness
· The bathroom layout forces twisting, stepping, or pivoting
Importantly, seated transfers are not only for non-ambulant clients. They are often the earliest safe alternative during functional decline.
Immediate vs Long-Term Solutions
Immediate (Risk Reduction) Solutions
Used when:
· There is an imminent fall risk
· The client is already experiencing failed transfers
· Funding timelines are uncertain
These include:
· Seated transfer systems that fit existing bathrooms
· Equipment that avoids structural modification
· Solutions deployable without waiting for building approvals
· Equipment that may be available using rent-to-buy options
Long-Term (Stability & Sustainability) Solutions
Appropriate when:
· The condition is progressive
· The home will remain the long-term environment
· Multiple daily transfers are required
Here, seated transfer pathways:
· Reduce cumulative injury risk
· Extend safe independent living
· Delay or prevent residential care escalation
The Showerbuddy SB1 was a saviour for this family
OT Documentation Language That Triggers Faster Approvals
Funding decisions increasingly hinge on risk language, not just function.
Language That Delays Approval
· “Client struggles at times”
· “Standing transfer becoming difficult”
· “May benefit from equipment in the future”
Language That Accelerates Approval
Use objective risk framing, for example:
“Client demonstrates inconsistent ability to achieve and maintain standing during transfers, creating an unacceptably high fall risk.”
“Standing transfers rely on carer physical intervention, increasing manual handling injury risk and breaching safe handling guidelines.”
“A seated transfer pathway is required to provide a predictable, repeatable transfer method that removes reliance on client weight-bearing.”
“Without a seated transfer solution, the risk of fall-related injury is high and immediate.”
Tip: Link the recommendation explicitly to risk elimination, not convenience or comfort.
Tie-In: Seated Transfer Pathways (SB1 / SB2-2T / SB3T)
Seated transfer systems such as SB1, SB2, SB2T and SB3T align directly with current funding priorities because they:
· Replace variable standing transfers with controlled seated movement
· Eliminate the need for lifting, pivoting, or stepping
· Fit within existing bathrooms, reducing modification costs
· Address both client safety and carer injury risk
· Provide a defensible, evidence-based alternative to standing transfers
For many clients, these systems are not a “later option”—they are the correct option once standing transfers become unreliable.
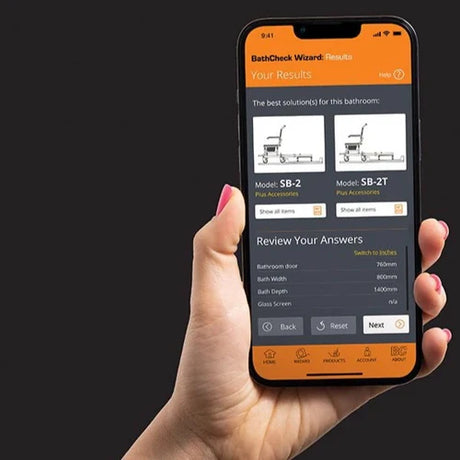
Practitioner Resources
To support OTs navigating increased scrutiny around standing transfers, this issue includes a set of practical, funding-ready resources you can download and use immediately.
These include a brand-neutral NDIS funding justification template, a separate version refined for Support at Home and other aged-care funding pathways, and an equipment suitability statement that sits outside the clinical justification to support procurement without compromising professional independence.
Each resource is designed to help articulate risk, justify the transition to seated transfer pathways, and streamline approval processes—particularly where time pressure and falls risk are escalating.
Download your resource
· Support at Home and Aged Care Funding Template
· Equipment Suitability Statement
Key Takeaway for OTs
The clinical question is no longer: “Can the client still stand?”
It is increasingly: “Is standing still the safest and most defensible transfer method?”
When the answer is no, seated transfer pathways are no longer optional—they are clinically indicated.
Coming Up Next in Access Insights
In the next issue, I’ll research the growing trend of rent-to-buy AT potentially helping with faster funding approvals.
Thank you for reading Access Insights.
My goal is to support therapists, and help clients stay safe at home — without the delays and confusion the system often creates. In researching this article and developing some images I also use AI.
Thank you for supporting Showerbuddy, the whole team is there to help you.
Barry Redican CEO — Showerbuddy
Contact us for any assistance … admin@shower-buddy.com
Safe access. Smart design. Real independence.
#NDIS #SupportAtHome #OT #Showerbuddy #AssistiveTechnology #AgedCare #BathroomSafety





























![Toilet Training A Young Child With Mobility Challenges [And How A Shower Chair Can Help]](http://shower-buddy.com/cdn/shop/articles/toilet-training-disabled-child_520x500_a90e5234-d372-435d-aa56-8da15dd3836c.webp?v=1722557239&width=460)



















